
 |
支气管扩张。反复感染导致瘢痕形成,它会在肺叶之间形成纤维性粘连。对于曾经有感染并累及胸膜的病人来说,纤维素性胸膜粘连比较常见。胸膜的广泛受累,可能出现胸膜腔闭塞。 Bronchiectasis is seen here. The repeated episodes of inflammation can result in scarring, which has resulted in fibrous adhesions between the lobes. Fibrous pleural adhesions are common in persons who have had past episodes of inflammation of the lung that involve the pleura. With extensive involvement, the pleural space may be obliterated. |
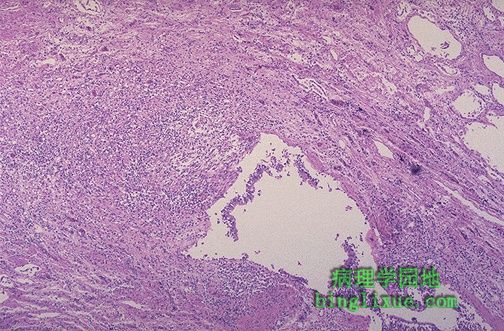 |
中下部显示扩张的支气管,由于坏死性炎症的破坏,粘膜和支气管壁不很清楚。这是支气管扩张的表现。支气管扩张不是特定的疾病,它是其它病变破坏气道的后果。 The mid lower portion of this photomicrograph demonstrates a dilated bronchus in which the mucosa and wall is not clearly seen because of the necrotizing inflammation with destruction. This is the microscopic appearance of bronchiectasis. Bronchiectasis is not a specific disease, but a consequence of another disease process that destroys airways. |
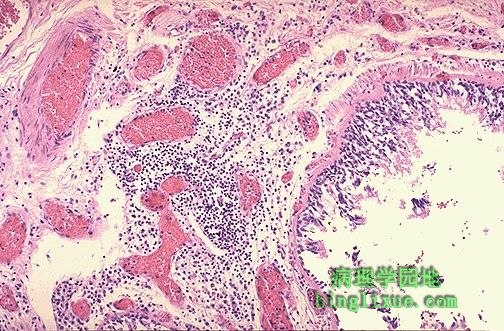 |
支气管粘膜下层有大量慢性炎细胞。 This photomicrograph demonstrates a bronchus with increased numbers of chronic inflammatory cells in the submucosa. Chronic bronchitis does not have characteristic pathologic findings, but is defined clinically as a persistent productive cough for at least three consecutive months in at least two consecutive years. Most patients are smokers. Often, there are features of emphysema as well. |
 |
肺气肿病人死后尸检胸腔被剖开,见肺表面数目众多的明显的肺大疱,是极度扩张的含气区,它从胸膜下膨胀起来。肺气肿具有典型的特征,肺泡被破坏,肺实质丧失,以致形成持久性的含气区增大。 The chest cavity is opened at autopsy to reveal numerous large bullae apparent on the surface of the lungs in a patient dying with emphysema.Bullae are large dilated airspaces that bulge out from beneath the pleura.Emphysema is characterized by a loss of lung parenchyma by destruction of alveoli so that there is permanent dilation of airspaces. |
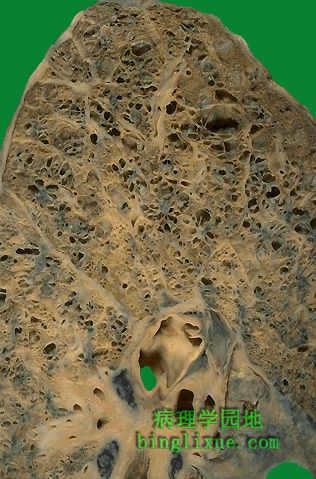 |
肺切面可见肺气肿扩张的含气区。重复感染致瘢痕形成,肺实质丧失,而不会纤维化。肺气肿主要有 2 种的类型: 腺泡中央型和全腺泡型。前者主要累及肺上叶,而后者则累及整个肺叶,尤其是肺底部。 On cut section of the lung, the dilated airspaces with emphysema are seen. Although there tends to be some scarring with time because of superimposed infections, the emphysematous process is one of loss of lung parenchyma, not fibrosis. There are two major types of emphysema: centrilobular (centriacinar) and panlobular (panacinar). The former involves primarily the upper lobes while the latter involves all lung fields, particularly the bases. Centrilobular emphysema occurs with loss of the respiratory bronchioles in the proximal portion of the acinus, with sparing of distal alveoli. This pattern is most typical for smokers.Panacinar emphysema occurs with loss of all portions of the acinus from the respiratory bronchiole to the alveoli. This pattern is typical for alpha-1-antitrypsin deficiency. |
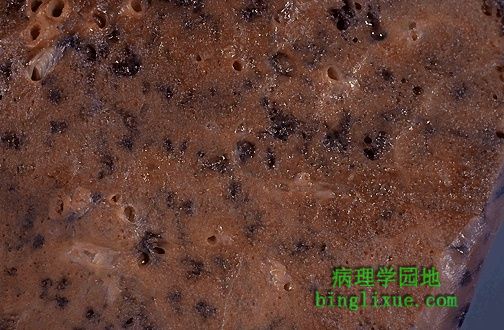 |
腺泡中央型在肺腺泡中央部分已丧失肺实质中出现一些“脏洞”,同时有炭尘色素沉积。此型多见于吸烟者。 This is a more subtle appearance for centrilobular emphysema in which there are "dirty holes" that appear focally where the central portions of lung acini have lost lung parenchyma while collecting anthracotic pigment at the same time. This pattern is typical for smokers. Smokers have a greater number of neutrophils and macrophages in their alveoli. Smoking irritates alveolar macrophages, which in turn release neutrophil chemotactic factors, such as interleukin 8, thus recruiting neutrophils. In addition, nicotine is chemotactic for neutrophils, and smoke can activate the alternative complement pathway (an inflammatory cascade). Proteases, particularly elastase, are secreted by these neutrophils and macrophages. Proteases are enzymes that are capable of digesting lung tissue and these chemicals are responsible for the damage seen in emphysema. Oxidants and free radicals in smoke also inhibit the alpha-1-antitrypsin circulating in the lung that protects alveoli from proteases. Chronic irritation by smoke also can lead to chronic bronchitis with excess production of mucus. Smoke interferes with the ciliary action of the respiratory epithelium and the mucus cannot be cleared. This predisposes the smoker to secondary and repeated infections. |
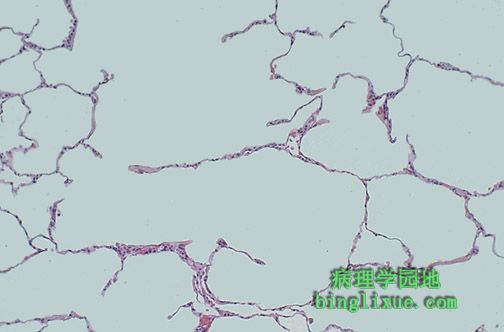 |
显微镜下,可看见肺气肿处的肺泡壁破坏。残留的含气区扩张。 Microscopically at high magnification, the loss of alveolar walls with emphysema is demonstrated. Remaining airspaces are dilated. |
 |
左肺肺动脉内大血栓。这类血栓多见于长期卧床病人的下肢深静脉或骨盆静脉。其它的不利因素包括四肢损伤、高凝状态(癌症病人患Trousseaus综合症;蛋白质 C 或 S 缺乏;使用口服避孕药),心衰,怀孕,年龄大。 Seen in the pulmonary artery to the left lung on cut section is a large pulmonary thromboembolus. Such thromboemboli typically originate in the leg veins or pelvic veins of persons who are immobilized. Other contributing factors include trauma to the extremities, hypercoagulable states (Trousseaus's syndrome in patients with carcinomas; protein C or S deficiency; use of oral contraceptives), heart failure, pregnancy, and older age. |
 |
鞍骑形栓子,栓塞于右肺动脉和左肺动脉交叉处。鞍状栓子是猝死原因。具有典型的外观。表面不甚规则,红褐色和灰白色交替出现,形状通常类似血栓所在静脉的轮廓。 Here is a "saddle embolus" that bridges across the pulmonary artery from the heart as it divides into right and left main pulmonary arteries. Such a saddle embolus is a cause for sudden death. This thromboembolus displays the typical gross appearance. The surface is somewhat irregular, and there are areas of pale tan to white admixed with dark red areas. The thrombus often has the outlines of the vein in which it formed. |
 |
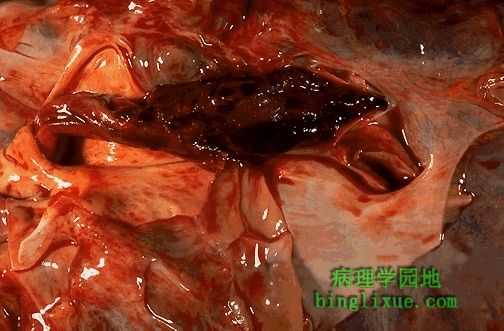
大血栓能引起死亡。中等大小的血栓(堵塞通向一个肺叶或一组肺叶的肺动脉)能产生如图所见的损害--肺出血性梗死,该病人得以幸存。梗死灶呈楔形,基底部位于脏层胸膜上。尽管携带大部分血和氧气的肺动脉被切断,但发自循环系统的分支动脉(供应肺大约1%的血)并没被切断,因此出血性梗死相对来说不易发生。 Large thromboemboli can cause death. Medium sized thrombomboli (blocking a pulmonary artery to a lobule or set of lobules) can produce the lesion seen here--a hemorrhagic pulmonary infarction, because the patient survives. The infarct is wedge-shaped and based on the pleura. These infarcts are hemorrhagic because, though the pulmonary artery carrying most of the blood and oxygen is cut off, the bronchial arteries from the systemic circulation (supplying about 1% of the blood to the lungs) is not cut off. |